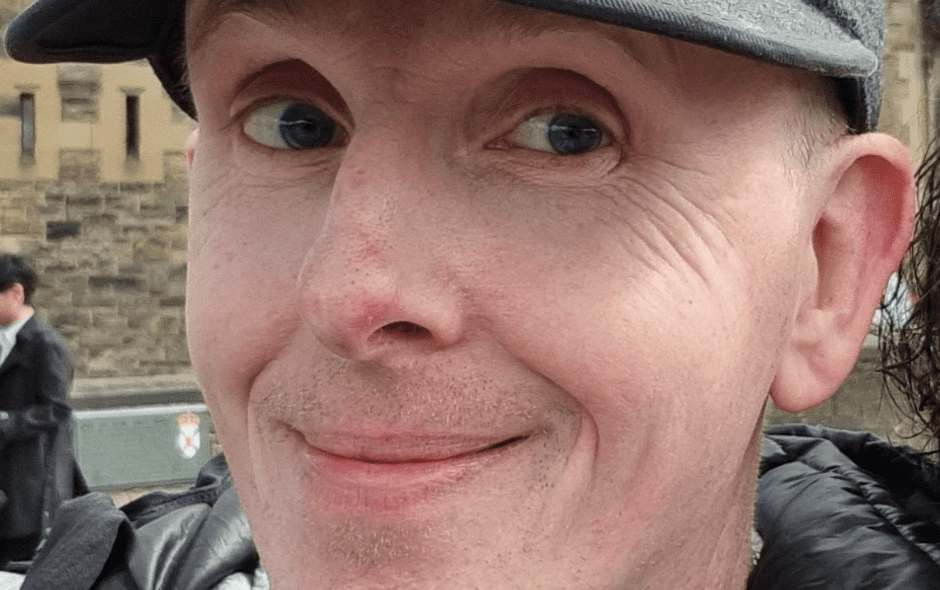
Bob was diagnosed with epilepsy when he was 18 years old. He shares how he felt when he was first diagnosed, how he manages his epilepsy while working full-time, and the importance of awareness days such as Purple Day.
When did you first get diagnosed with epilepsy?
I was diagnosed when I was 18 so it has been 30 years since my diagnosis. I always knew something wasn’t right and could not verbalise what was happening to me.
My mother once advised me that on a school report, a teacher had put “Robert tries very hard but is a bit of a daydreamer.” Little did we know that the teacher was on to something.
Diagnosis 30 years ago was a lot different from this generation, we had been through a number of different theories and suggestions before they could definitively say it is epilepsy.
How did you feel when you were first diagnosed?
Initially, I was glad to have an answer of sorts but then having that label and the stigma that was associated with the “epilepsy” label back then was not positive.
I was not really aware of the profound change that this was going to have on my life moving forward.
The many different medications, the restrictions that were then in place eg…never being able to drive, the impact of my social circle and their reaction, and the many battles that were then ahead that I was not and could not be prepared for.
What type of seizures do you have? How does it affect you?
The names have changed over the years but I refer to them as simple partial (focal seizure), complex partial (focal impaired awareness seizure), and generalised (tonic/clonic) seizures.
They have varied in type and frequency over many years. In my earlier years, they were predominantly simple partial where I had awareness but couldn’t communicate something was happening and would wear off after a while.
Occasionally a major typical tonic-clonic seizure would occur which would sometimes result in injury or hospitalisation.
The complex partial seizures started in 2005 and are very scary due to the lack of awareness.
I could be walking down the street have a complex partial seizure and then start walking down the middle of the road without any awareness of what was happening, try explaining that to a police officer or member of the public.
After a seizure like this, my recall of the event and sometimes hours prior to the seizure was no longer available as if someone just took a few hours of my life and erased them.
These were the worst for me, at least with a typical seizure normally involves a fall, an injury, and recovery but impaired awareness ones can lead to scary situations.
In 2015 during it was also suspected that I was also being impacted by Non-Epileptic Attack Disorder (NEAD) as well as the other seizure types which again I found have stigmas of their own.
This was a period of time of poor mental health and poor seizure control and required specialist intervention.
What challenges have you faced since being diagnosed with epilepsy?
The challenges are in everyday life but mainly I have found a lot of challenges are personal with your own routines, health, and discipline regarding self-care and minimising triggers.
It can often be a fight with yourself that you need to win before any external factors are considered.
The harsh reality of challenges has been mainly in every work environment that I have ever worked in.
The necessity to become an expert with regards to the Equality Act says a lot for employers in the Uk and often having to educate employers and their managerial staff over many years has been a major challenge.
This has thankfully not been the case in all circumstances and after many years of struggles and different, difficult, distressing situations I currently have an element of workplace stability, and reasonable adjustments in place and I am healthier for it, my seizure frequency is healthier for it and my performance as an employee is healthier for it.
As for dealing with the DWP, well that is another story!
We always say that epilepsy is more than seizures. Do you feel this has been your experience?
Absolutely if anything I sometimes feel that seizures are the easy part. The impact of medication side effects can impact people in many ways especially if they are on a combination of medications.
The experience of trying many different combinations of up to 12 anti-epileptic medications over many years has been a challenge.
Epilepsy can impact your recall, long and short-term memory, the ability to find words and communicate can be impacted, and the ability to read, write, spell, type, and multi-task to a degree can be impacted.
The speed of processing can be impacted either by seizures or medication or both and I suspect there is a cumulative impact as well if you have taken seizures for many years.
The actual fact that you know that your intellect may be fully intact but your capacity and speed of processing is lower or slower is very frustrating and also difficult to explain to some people who have their own perception of what epilepsy is.
The impacts of sleeping patterns which if not managed can then be seizure triggers have been a major challenge for me.
The physical impacts and injuries, broken bones, and dental damage come with the territory but there is a 1000% correlation between epilepsy and mental health illnesses like anxiety, depression, etc.
How have you managed your epilepsy and also work full time? What support have you received from your employer?
After many years of trying and often failing miserably, I have found that for me routine is everything.
Eating at regular times, sleeping at regular times, and taking medication at regular times are key to seizure management.
Having a structured day where these things are managed has been a key factor. If anything epilepsy has taught me discipline and also to stand up for myself, believe in myself, and fight my corner.
Without going into detail I now work a fixed shift, with fixed breaks where I can eat, take medication, and check in with family.
Working from home, I now have workplace adjustments in place and safety protocols in place (eg. Telecare) that allow me to function as an effective employee and be free from the stigma that many other people still have to endure and are still fighting to be free from.
How important do you think awareness days like Purple Day are?
Anything that shines a light of awareness on epilepsy is key to getting the message across.
During the lockdown period when I was not sleeping well, I joined in the Facebook or Instagram live sessions that Cassidy Megan held even at 2am.
The fact that there are so many different types of epilepsy and so many different personalised scenarios and that it is perhaps the most frequently diagnosed neurological illness yet appears to be severely underfunded on the surface and under-promoted by media means that all forms of awareness days, events, etc are more important more than ever.
What would you say to others who have been recently diagnosed with epilepsy?
I would advise to reach out to epilepsy organisations, charities, and groups and ask the questions you want to ask and educate yourself about your diagnosis.
The best way to treat your epilepsy is to understand it. This is not a 30-minute job and in some cases a 30-year job.
What works for other people will not always work for you but if you never try, you’ll never know.
Become familiar with regards to your rights and other people’s responsibilities towards you whether that be GP, Consultants, DWP, employers, etc.
You are still worthwhile, your diagnosis doesn’t define you but your actions and your love for yourself and those around you will.
If you would like to share your experiences of living with epilepsy, please email David Coates our Communications Officer at dcoates@epilepsyscotland.org.uk or call 0141 427 4911.